Jumper's knee
Synonym: Patellar tendinitis
Table of contents
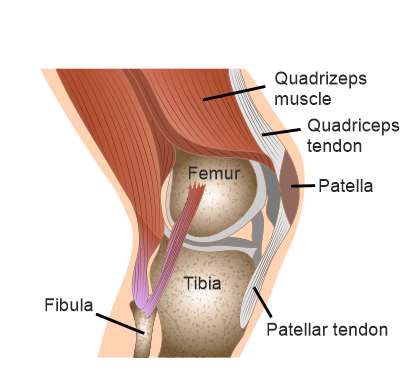
Systematics of the patella and patellar tendon
The patellar tendon is actually a ligament (ligamentum patellae) that connects the lower tip of the kneecap to the tibia. It can be considered the lower continuation of the tendon of the large knee extensor (quadriceps tendon). The quadriceps tendon radiates extensively into the anterior surface of the patella, but only uses it as an intermediate attachment. At the lower pole of the patella, it then merges with the patellar tendon, which finally attaches to the front of the tibial head. When the quadriceps are tensed, a tensile force is created that is transmitted via the patella and patellar tendon to the tibial head and results in an extension of the knee joint. The extension in the knee joint enables us to perform movements such as jumping or standing up from a squatting position.
What is jumper's knee?
Jumper's knee is a painful disease of the patellar tendon insertion (insertion tendinopathy) in the area of the lower patellar pole. The condition is usually the result of chronic overuse of the patellar tendon and therefore often occurs in sports that involve forced knee joint extension. This applies primarily to sports that are particularly jump-intensive or that require a constant abrupt change of direction (basketball, volleyball, football, handball or track and field). Jumper's knee is very common in competitive athletes (up to 40% in professional basketball and volleyball players).
How does jumper's knee develop?
The exact mechanisms that cause the painful changes in the patellar tendon have not yet been clarified in detail. However, it is now known that the cause of the disease is not, or only to a limited extent, inflammation, but that degenerative changes in the patellar tendon at the tendon-bone transition at the lower patellar tip are responsible for the pain. This was confirmed by microscopic examinations of small tissue samples (biopsies) of damaged patellar tendons in patients diagnosed with jumper's knee. These showed tissue changes with tiny tears and injuries (microruptures) of the tendon fibres on a cellular level and degenerative deposits of connective tissue material (chondromucoid deposits). In addition, an increased presence of tendon cells with abnormal activity could be detected, which, with the release of various messenger substances and enzymes, are responsible for a pathological formation of small blood vessels and damage to the tendon fibres. These findings in connection with the fact that no inflammatory cells could be detected in the microscopic examinations clearly speak for a chronic overload of the patellar tendon and thus a degeneration as the primary cause of the jumper's knee. The term tendinitis (inflammation of the tendon) should therefore be disregarded and replaced by "tendinopathy". This insight is of great importance for the choice of the optimal therapy.
However, jumper's knee can also occur in patients who are not active in competitive sports. In some studies, it was found that jumper's knee is also based on a certain impingement problem - i.e. a jamming of the patellar tendon in the area of the lower patellar pole. Two variants of impingement can be described:
- Pinching at the lower patellar pole
Since not all tendon fibres of the patellar tendon attach exactly to the lower patellar tip, but some also radiate into the patellar anterior surface, the middle area of the patellar tendon can become pinched at the lower patellar pole when the knee joint is bent.
- Pinching in the lateral part of the gliding groove on the thigh bone (femur).
The patella forms a joint with the femur (patellofemoral joint). The back surface of the patella is covered with cartilage, which ensures low-friction sliding in a groove of the femur (trochlea femoris). If some of the tendon fibres from deeper layers of the patellar tendon also radiate into the back surface of the patella, these fibres are trapped between the patella and the lateral part of the femoral sliding groove.
In both cases, there is continuous irritation of the patellar tendon with pain at the lower tip of the patella without the patient being overly active in sports. The cause of jumper's knee in these cases would be purely anatomical and one speaks of a predisposition (susceptibility) of the patient to this condition. Other anatomical influencing factors would be, for example, the patella alta or a congenital ligament weakness (ligament laxity).
Symptoms of jumper's knee
Jumper's knee is characterised by easily localisable load-dependent anterior knee pain at the lower pole of the patella. The characteristic pain manifests itself mainly during the exercise of the above-mentioned sports, whereby the pain intensity usually increases sharply without prior performance of adequate warm-up exercises. As the disease progresses, some patients also experience onset pain, which in more severe cases is accompanied by redness, swelling or oedematous distension of the surrounding tissue. In higher stages of the disease, everyday movements (e.g. climbing stairs, carrying heavy loads) and extending the knee joint against slight resistance are also painful. The disease is characterised by a chronic course and often develops over months to years.

Diagnosis of jumper's knee
The diagnosis of jumper's knee is primarily made after clinical examination. For further assessment of the severity of the disease, or if the clinical examination is unclear, additional image-diagnostic (radiological) procedures are used.
Clinical diagnostics
The clinical diagnosis includes a detailed discussion with the patient (anamnesis), which provides initial indications of the underlying disease. This is followed by the clinical physical examination, in which the characteristic symptoms are specifically sought out and which should confirm the suspicion of jumper's knee. The patient is in a relaxed supine position on the examination bed during the entire examination. First, the pressure pain of the patellar tendon insertion at the kneecap is determined by light finger pressure on the lower patellar pole. At the same time, the doctor can check the surrounding tissue for any swelling, induration, overheating or redness. The patient is then asked to bend the legs and stretch them out again against moderate resistance from the doctor. Pain provocation during this examination technique would also provide an indication of jumper's knee.
Diagnostic imaging
Various imaging (radiological) procedures are available for further clarification. In this case, magnetic resonance imaging (MRI) is of the greatest importance. In chronic forms, MRI can be used to evaluate the severity of the disease very well, as the images provide important information about the quality of the patellar tendon. Here, one explicitly looks for any partial tears (partial rupture), thickening, calcification or ossification of the patellar tendon attachment to the kneecap. Occasionally, due to chronic irritation, bone marrow oedema at the lower tip of the patella and swelling of the surrounding tissue become noticeable in the MRI. All this information makes it possible to accurately classify jumper's knee (see below) into different stages. In this way, the therapy procedure can be optimised, adapted to the respective degree of severity and the healing process of the disease.
Ultrasound examination is a quick and uncomplicated way of detecting tissue changes in the area of the patellar tendon insertion. However, it can in no way replace MRI findings, as it can only provide information about the presence of swelling, oedema or the general condition (homogeneity) of the surrounding tissue and, conditionally, the patellar tendon.
The usual X-ray of the knee joint is of secondary importance for the diagnosis of jumper's knee. However, it can be used to exclude diseases that cause similar symptoms (Osgood-Schlatter disease, Sinding-Larsen-Johansson disease).
Classification of jumper's knee
The information obtained from the patient interview, clinical physical examination and imaging allows the classification of jumper's knee into 5 stages [1]:
- Pain after exertion
- Pain during and after exercise
- Pain before and after exercise (persistent pain)
- Partial rupture of the patellar tendon
- Complete rupture of the patellar tendon
The level of the stage correlates with the severity of the disease and determines the further course of therapy.
[1] Classification according to Blazina 1973, modified by Biedert 1997
Diseases with similar symptoms (differential diagnoses)
Often, the diagnosis of jumper's knee is clear on the basis of the clinical findings. However, there are a number of other orthopaedic conditions that can cause similar symptoms:
- Osgood-Schlatter disease
Painful irritation of the patellar tendon insertion at the head of the tibia due to overloading with potential detachment of bone fragments and subsequent osteonecrosis, which can be seen on X-ray. The pain occurs somewhat further down than in jumper's knee.
- Sinding-Larsen-Johansson disease
As in jumper's knee, the patellar tendon insertion at the lower pole of the patella is affected. However, pieces of bone also detach from the patella and subsequently die (osteonecrosis). The disease can be seen in an X-ray.
- Stress fractures
- Inflammation or impingement of the Hoffa fat body
The Hoffa fat body is located directly behind the patellar tendon and can also be pathologically altered as an accompanying symptom of some knee joint diseases. Sometimes inflammation or impingement of the fat body can cause symptoms similar to those of jumper's knee.
- Bursitis praepatellaris
- Retropatellar chondropathy (cartilage damage or wear behind the kneecap)
Therapy of jumper's knee
In principle, conservative and surgical therapy methods are available for the best possible healing. Extracorporeal shock wave therapy (see below) is a particularly effective method of treating the disease conservatively. Patients in the first and second stages of the disease primarily receive conservative therapy. In stages III and IV, surgery can also be performed, depending on the clinical status, age and performance level of the patient. The fifth stage requires surgical intervention in any case.
Conservative therapy
- Rest and abstinence from sports
In the beginning, the patient is advised to take it easy and to abstain from the triggering sport. Should the patient nevertheless remain active in sports, it is recommended to carry out a targeted warm-up training with stretching exercises before the training session.
- Pain medication
If pain occurs, cold application, ointments and anti-inflammatory painkillers (NSAIDs) can relieve the symptoms. However, these do not help to cure jumper's knee because the cause is not inflammation (see above).
- Physiotherapy
Targeted physiotherapy exercises focusing on the quadriceps (knee extensors) and "hamstring" (knee flexors) can significantly improve the course of the disease.
- Extracorporeal shock wave therapy (ESWT)
ESWT plays a special role in the therapy of jumper's knee. As in an ultrasound examination, the head of a specific device filled with water is pointed at the affected region. The device then generates shock waves with increasing energy, which is transmitted via the water-filled head to the tissue under the skin. Several studies have shown that these shock waves have a positive effect on the affected tissue (in this case the patrol tendon). This is expressed in the sense of increased blood circulation, formation of growth factors, new tissue formation and regeneration, better wound healing and even relief of pain. The procedure is a good alternative to surgery and has only a few side effects such as slight pain during the procedure, redness or the formation of a haematoma in the affected area.

Surgical therapy
In very severe forms of jumper's knee, surgery may also be considered. The degenerative tissue is isolated either arthroscopically or by open surgery. In the case of a partial rupture, the patellar tendon is reinforced, and in the case of a complete rupture, it is reconstructed. The healing process after surgical therapy is very protracted and can take up to 6 - 12 months.