Meniscus transplantation/meniscus replacement
Synonyms: Meniscus allograft transplantation (MAT), meniscus scaffold replacement (MSR)
Table of contents
- Anatomy and function of the meniscus
- Why is a meniscus transplant/ replacement necessary?
- What distinguishes meniscus transplantation from artificial meniscus replacement?
- Meniscus Allograft Transplantation (MAT)
- Artificial meniscus replacement (Meniscus Scaffold Replacement - MSR)
- When is a meniscus transplant/artificial meniscus replacement used?
- Results after meniscus transplantation/ artificial meniscus replacement
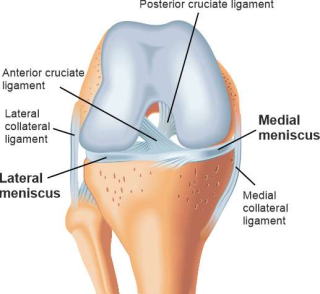
Anatomy and function of the meniscus
The meniscus is a crescent-shaped structure made of fibrocartilage that performs a shock-absorbing function in the knee. A distinction is made between an inner and outer meniscus. Both are anchored to the surface of the shinbone (tibial plateau) by two ends each, the so-called meniscus roots. This is to allow the menisci to move and adapt well during movements in the knee joint.
Why is a meniscus transplant/replacement necessary?
A (partial) meniscus removal is a very common orthopaedic intervention that becomes necessary due to a meniscus injury or damage. Even if an experienced surgeon takes care to preserve the meniscus (e.g. by suturing), this is only possible under certain conditions. Even a small loss of meniscus substance leads to a strong increase in the pressure load on the joint cartilage, as the shock-absorbing and force-distributing function of the meniscus is reduced. This leads to faster joint wear (arthrosis). For this reason, total or subtotal removal of the meniscus is a common cause of persistent discomfort (postmeniscectomy syndrome) and progressive arthrosis. Arthroscopic meniscus transplantation is a minimally invasive method to restore the natural function of the meniscus and normalise the pressure conditions in the joint by increasing the contact area of the joint partners in the knee. This should subsequently slow down the progressive wear and tear of the joint.
What distinguishes meniscus transplantation from artificial meniscus replacement?
The two methods differ in terms of the areas of application and the surgical techniques and are described in more detail below.
Meniscus Allograft Transplantation (MAT)
In meniscus allograft transplantation, the entire meniscus is replaced by a donor preparation (allograft). This has the advantage that the biological and biomechanical condition of the meniscus is almost exactly the same as the original condition. Allograft means that the transplant - in this case the meniscus - comes from a human donor. The meniscus is removed from the donor under sterile conditions and then specially processed and stored in a certified tissue bank. In contrast to organs, there is no rejection reaction with meniscus, tendon or bone tissue. Accordingly, no special medication is necessary after the meniscus transplantation.
Before the meniscus transplantation, the knee is precisely measured using X-rays or an MRI, as the transplanted meniscus may only vary slightly in size from the body's own meniscus. Only when a suitable meniscus has been found can the operation be performed.

Surgical technique
Meniscus transplantation can be performed arthroscopically. A distinction is made between pure soft tissue fixation of the meniscus graft and fixation with bone blocks.
In the case of bone block fixation, the meniscus together with its bony anchorage to the meniscus roots is inserted into a previously prepared bony bed at the recipient's site.
In soft tissue fixation, the meniscus graft is fixed to the joint capsule using special suturing techniques. The meniscus roots are inserted into bony drill channels in the tibia to allow for bony healing. This allows good adaptation of the donor meniscus with the least possible invasiveness. The surgical method requires a high level of experience and technical expertise on the part of the surgeon, but can avoid the need for open knee surgery with all the accompanying surgical risks.
Artificial meniscus replacement (Meniscus Scaffold Replacement - MSR)
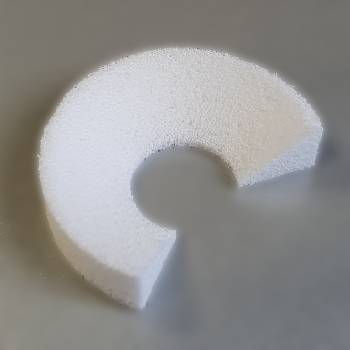
The use of an artificial meniscus (so-called scaffold) requires that the meniscus roots and a meniscus rim are still intact. This is most often the case after a partial removal of the meniscus. Since this poses the risk of rapid cartilage wear, this is the main area of application for meniscus replacement.
In Europe, two different products are used that are supposed to resemble the biomechanical properties of the original meniscus. One is called CMI and is made of type I collagen, the other is called ACTIfit and is based on porous polycaprolactone and urethane segments that aim to allow the body's own tissue to grow into it. Both preparations are acellular. This means that no cells are present in the material at the time of implantation. Over time, the scaffolds dissolve by themselves and are replaced by the body's own tissue.
Surgical technique
Meniscus replacement surgery can also be performed arthroscopically. However, it does not require any complex preparations, as the defect in the meniscus is measured during the operation and the artificial meniscus is cut to size and adapted to the defect while still in the operating theatre. The artificial preparation is fixed by attaching it to the remnants of the body's own meniscus using special suturing techniques. Compared to meniscus transplantation, meniscus replacement surgery is less complex because no bony drilling channels are necessary.
When is a meniscus transplant/artificial meniscus replacement used?
The field of application of meniscus transplantation (MAT) differs in some areas from artificial meniscus replacement (MSR). However, the main goal of both operations is to improve complaints and, in the best case, to slow down or delay joint wear (arthrosis) in the knee joint.
The largest area of application for meniscus transplantation, in which the best results are also described, is ideally found in a young patient with symptomatic loss of the medial or lateral meniscus without the simultaneous presence of pronounced degenerative changes (arthrosis) in the knee joint. A previous meniscus operation in which large parts of the meniscus were removed and there is a clear risk of rapidly progressing arthrosis can also be a criterion for a meniscus transplant. In recent years, the indications for meniscus transplantation have been expanded, as studies with older patients and higher-grade cartilage lesions showed good clinical results, although the survival rate of the transplanted meniscus was lower. It is advisable to assess each patient individually and to focus on biological age rather than purely on date of birth. Accompanying pathologies such as circumscribed cartilage damage, instabilities or axial misalignments should in any case be treated surgically in order not to worsen the postoperative results and the survival rate of the meniscus transplant.
In principle, the same indications apply for meniscus replacement as for meniscus transplantation. However, the prerequisite for meniscus replacement is that the meniscus roots and the outer meniscus rim have remained intact.
Results after meniscus transplantation/ artificial meniscus replacement
Current studies show that after meniscus transplantation there is a significant improvement in complaints in most patients, provided that the area of application and the exclusion criteria are taken into account. This can be understood as an effective reduction in pain, as well as a general improvement in knee joint function and thus ultimately also in the quality of life. Meanwhile, 5-10 year graft survival rates of 85.8% for the medial meniscus and 89.2% for the lateral meniscus have been described.1
At the moment, scientists are intensively studying the potential areas of application of meniscus transplantation. Studies repeatedly show that meniscus transplantation can also make sense in cases of higher-grade cartilage damage. Furthermore, there is evidence that meniscus transplantation can reduce the progression of osteoarthritis, although not as effectively as the patient's own meniscus.
Very good results were also observed for the implantation of an artificial meniscus for the preparations CMI and ACTIFIT when used appropriately. Among other things, the patients described a significant reduction in pain, as well as improved knee joint function and thus an overall increase in quality of life.
1 Bin SI, Nha KW, Cheong JY, Shin YS. Midterm and long-term results of medial versus lateral meniscal allograft transplantation: a meta-analysis. Am J Sports Med 2018;46:1243–1250.