Knee replacement, knee prosthesis
Synonyms: knee arthroplasty, artificial knee joint
Table of contents
- What is a knee replacement?
- When is a knee replacement necessary?
- What are the different knee replacement implants?
- Partial (unicompartmental) replacement
- Total knee replacement/arthroplasty - TKA
- What is the procedure for knee replacement surgery?
- Aftercare for a knee replacement
- What complications and risks can occur during knee replacement surgery?
- Loosening of the knee replacement
- How long does a knee replacement last?
- What results can one expect from a knee replacement?
- Which knee replacement can be considered for a nickel allergy?
What is a knee replacement?
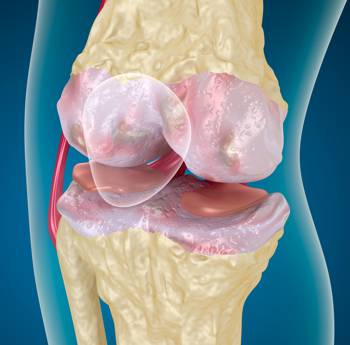
A knee replacement is the artificial replacement of a diseased knee joint. The diseased parts of the joint are removed during an operation and replaced with artificial implants. Depending on the extent of the osteoarthritis, either the entire knee joint can be replaced (total knee arthroplasty - TKA), or a partial replacement of the more severely affected part of the joint can be carried out (half-slide, patellofemoral sliding bearing prosthesis). As a rule, knee replacements are made of specially manufactured metal alloys.

The destroyed joint components (cartilage sliding surfaces) in the contact area between the femur and the tibia are replaced by metallic surfaces and anchored in the bone. This results in a femoral component and a tibial component of the prosthesis. To prevent metal from rubbing against metal during movement, the tibia component has a so-called "inlay" made of a special plastic (highly cross-linked polyethylene) as an additional sliding body. This is a relatively soft plastic material that is also found in other forms in plastic bottles (PET), and its excellent elasticity significantly improves the movement of the knee. It can be compared in a broader sense to the function of the meniscus in the healthy knee.

When is a knee replacement necessary?
If other treatment methods are unsuccessful, the surgical implantation of a knee replacement is usually the last treatment option for advanced knee arthrosis. Since osteoarthritis is a chronically progressive joint wear disease, the cartilage wear or the cartilage defect can become so extensive that no improvement in the symptoms can be expected from purely conservative therapy. [If, for example, a patient with severe knee osteoarthritis continues to have symptoms or even experiences an increase in symptoms despite physiotherapy and attempts at "cartilage-building" therapy (hyaluronic acid infiltration, ACP therapy), a knee replacement must be considered for this patient. Important criteria for a knee replacement are the occurrence of pain at night and at rest, significantly reduced mobility in the knee joint, as well as all associated complaints that can impair pain-free coping with everyday life. Such a clinical picture is shown in X-rays by a massive narrowing of the joint space or in MRI usually in the form of high-grade cartilage damage (chondropathy grade III-IV). This means that the cartilage is already worn down to (close to) the bone and thus its protective and gliding functions are no longer guaranteed. Imaging together with clinical diagnostics provides the orthopaedic surgeon with the necessary information to decide on the further procedure and the choice of the right knee replacement. The individual symptoms of the patient are of particular importance.
What are the different knee replacement implants?
The knee is a compound joint consisting of three joint bodies (patella, femur and tibia), which form two joints between them. Between the patella and the thigh bone (femur) is the patellofemoral joint, and between the thigh bone and the shin bone (tibia) is the tibiofemoral joint, which can be further divided into an inner (medial) and an outer (lateral) section. Depending on which or how many joint sections are affected by the osteoarthritis, a partial (unicompartmental) knee replacement or a total knee replacement can be used.
Partial (unicompartmental) knee replacement
Unicondylar knee replacement
If only the middle (or outer) compartment of the tibiofemoral joint is damaged in isolation by the osteoarthritis process (e.g. in the case of bow-leg or knock-kneed deformity), a half-slide prosthesis can be considered after precise evaluation of the joint status. The advantage of such a partial prosthesis is that by preserving both cruciate ligaments and only minimal damage to the capsule-ligament apparatus, the body's own depth sensitivity and stability of the knee joint is largely preserved. Current studies show that patients who are eligible for and receive a unicondylar knee replacement can have better mobility in the knee joint after surgery than patients who were fitted with a total knee replacement. The fact that knee replacements are constantly being modified and improved contributes to this. In addition, the prosthesis components are all available in different sizes so that an individual fitting can be made to the joint bodies. This means that only as much joint surface (bone) is removed as is actually replaced by the knee replacement. As with total knee replacement, the joint surfaces of the femur and tibia are replaced with metal. A polyethylene inlay is also attached to the tibia component of the prosthesis, on which the metal can slide optimally. The prosthesis is usually cemented to the bone to prevent early loosening. Although some study authors describe a survival rate of up to 98% for the unicondylar prosthesis after ten years, partial prostheses tend to have a reduced durability compared to total endoprostheses.


Patellofemoral replacement
The patellofemoral partial prosthesis can be used for isolated osteoarthritis in the joint between the kneecap and the femoral gliding bearing (patellofemoral osteoarthritis). The sustainability and effectiveness of this prosthesis is only given if numerous prerequisites are met and under certain conditions. Implantation of the patellofemoral prosthesis requires a high degree of experience and should only be performed by a knee specialist after thorough examination and clarification of all potential exclusion criteria. The advantage of such an operation is that the arthrosis process - if limited to the patellofemoral joint - spreads more slowly to the large compartments of the tibiofemoral joint due to the patellofemoral prosthesis. Timely application of such a prosthesis can therefore significantly delay the date for total knee arthroplasty. One option for implantation is the HemiCAP prosthesis, which is screwed firmly into the thigh bone as a sliding bearing replacement. It is available in different sizes and shapes to match the natural shape of the gliding groove. Precise selection of the right size is essential for the result. If there is no cartilage damage on the back surface of the patella, the body's own cartilage can be retained as a gliding partner. Otherwise, a highly cross-linked polyethylene inlay is placed behind the patella as a joint partner.


Total knee replacement/arthroplasty - TKA
With the TKA, both the femoral and the tibial joint surfaces of both tibiofemoral joint compartments are completely replaced by the metal prosthesis. Thus, on the one hand, there is a femoral component of the knee replacement that reproduces the paired, cylindrical ends of the femur and also has a sliding groove for the kneecap on the front side. On the other hand, the tibial component replaces the so-called "tibial plateau" of the tibia and is firmly anchored in the tibia via a stem. The polyethylene inlay is also attached to the tibial component of the knee replacement, which is intended to allow low-friction sliding in the knee joint during movement. Modern total knee replacements are so-called surface replacement prostheses, in which only the superficial damaged joint surfaces (cartilage) are removed and replaced by the knee replacement. The underlying bone remains largely intact. In certain cases, the cartilage on the kneecap can also be replaced by a patellar component of the knee replacement. In this case, the broken cartilage is removed and replaced with slippery polyethylene.


In total knee replacement, one often comes across the terms "coupled" and "uncoupled" prosthesis. These terms refer to the possibilities of movement in the knee joint. From a mechanical point of view, the knee joint is often incorrectly referred to as a hinge joint. A hinge joint has only one degree of freedom, which in the case of the knee would mean that only flexion and extension would be possible in the knee joint. However, when the knee is flexed, the lateral ligaments slacken, which also allows rotation in the knee joint. So if the medial and lateral collateral ligaments and the posterior cruciate ligament are intact, an uncoupled knee replacement is used, which is closest to the natural function of the knee. Stabilisation is still provided by the aforementioned endogenous ligaments and rotation is possible in addition to extension and flexion. Since all components of the uncoupled knee replacement remain mobile, the uncoupled knee replacement is less stressed and is characterised by a longer durability.
The coupled knee replacement firmly connects the upper and lower leg components of the prosthesis and only allows extension and flexion in the knee joint but without rotation. It thus imitates the mechanics of a hinge joint. The coupled knee replacement is used when the body's own collateral ligaments or the cruciate ligaments are no longer effective (e.g. in extreme knock-kneed or bow-legged deformity). The ligamentous apparatus would not be able to stabilise an uncoupled knee replacement and the risk of dislocation would be drastically increased. The comfort of movement and the durability of a coupled knee replacement cannot be compared with an uncoupled one. Therefore, an uncoupled knee replacement is used nowadays whenever possible.
What is the procedure for knee replacement surgery?
Before the operation, special X-rays are taken of the knee and the whole leg in order to plan the operation and the implants precisely. The anaesthesia can be either a general anaesthesia (general anaesthesia) or a spinal anaesthesia (cross stitch).
In the operating theatre, the patient is in a supine position. The incision is usually made longitudinally in the centre, from the base of the patellar tendon to slightly above the upper edge of the patella. After opening the joint, the patella is pushed to the side to gain insight into the tibiofemoral joint. Subsequently, the diseased articular cartilage with a piece of underlying bone is removed using a saw gauge with an oscillating saw. In order to ensure a firm fit of the knee replacement, the size of the implant is precisely adapted to the patient and fixed to the cut surfaces of the bone. There are knee replacements that are fixed with quick-bonding bone cement as well as cementless prostheses using the "press-fit" method. Another option is the hybrid fixation, where the femoral component is cemented and the tibial component is attached using the "press-fit" method. The stability and mobility of the knee replacement are checked by the surgeon while the operation is still in progress, by moving the knee thoroughly.
Aftercare for a knee replacement
Rapid Recovery
After the operation, a hospital stay of about 5-7 days is to be expected, during which the patient should become pain-free and mobile again as quickly as possible through intensive follow-up treatment and care. A proven concept practised at the Orthopaedic Hospital Speising is the so-called Rapid Recovery Programme. From the first day of hospitalisation, the patient is informed in the best possible way about the entire process, about all therapeutic measures and about what to do after discharge (patient training). To ensure that the patient is also optimally supported at home, an accompanying person can be present when the information is given. Directly after the operation, the patient is closely monitored in the recovery room until he or she is medically stable and pain-free, which is ensured by the choice of the ideal post-operative pain therapy. Afterwards, the qualified nursing staff accompanies the patient to the room, where the first attempts at mobilisation are practised with the physiotherapy and occupational therapy specialists on the very first day. For example, getting up slowly and putting on clothes independently should be practised under professional supervision. During the following days in the hospital, the patient continues to be cared for by the therapists and practises climbing stairs independently with 2 forearm crutches. After the hospital stay, individual physiotherapy continues and intensive work is done on regaining mobility during a 3 - 4 week rehabilitation stay in a specialised centre. At the Orthopaedic Hospital Speising it is also possible to complete the rehabilitation on an outpatient basis.
Controls after the surgery
X-ray checks of the knee replacement are still carried out during the operation and the hospital stay to check the correct position. X-rays are also taken after the rehabilitation phase has been completed, as the knee is subjected to intensive stress here. Further X-rays should be taken six months after the operation and then at 1 - 2 year intervals, or at any time when complaints occur.
During regular clinical checks, it is important to follow the movement status of the joint and also to be able to recognise signs of infection or other complications in good time so that the right countermeasures can be taken at an early stage.

What complications and risks can occur during knee replacement surgery?
Like any other surgical intervention, the implantation of a knee replacement can involve risks. The fact that the knee joint is surgically opened creates an entry point for various germs. There is therefore a risk of joint infection. To minimise this risk, the patient is given antibiotics during the operation. Another risk is the development of thrombosis, which is to be prevented by blood-thinning medication after the operation. A pathological wound healing and scarring process with proliferation of scar tissue after knee surgery can lead to so-called arthrofibrosis. While mobility in the knee gradually improves in normal cases, arthrofibrosis causes progressive movement restrictions.
Loosening of the knee replacement
In principle, a distinction is made between septic and aseptic loosening. The former is caused by a bacterial infection of the knee joint in which a bacterial film is deposited over the implant. The resulting immune response leads, among other things, to bone loss (osteolysis) and the knee replacement loosens. Such an infection requires immediate action and the administration of antibiotics. In the worst case, the knee replacement must even be removed to treat the joint infection and a revision endoprosthesis inserted at a later date.
Aseptic loosening can occur when the knee replacement has passed its expiry date. The continuous application of force to the polyethylene inlay can cause abrasion particles to be released, which trigger an immune reaction in the knee. However, the immune macrophages cannot break down these particles, which means that the immune reaction does not decrease or even gets worse. The result is bone loss around the implant, which causes the knee replacement to come loose.
A loose knee replacement cannot withstand the high shear and pressure forces that occur when walking and standing, and usually has to be replaced by a revision prosthesis.
How long does a knee replacement last?
The survival time of a knee replacement varies greatly and depends on various factors. If the operation and post-operative management are free of complications, one can expect a durability of about 15 - 20 years. Body weight, the amount of weight bearing, bone quality, diet and general lifestyle are factors that can influence durability.
If the plastic inlay wears down over time, it can be replaced. If there are increasing signs of loosening of the knee replacement and resulting discomfort, the prosthesis can be replaced with a so-called revision knee replacement. However, this procedure is more complicated and associated with a higher risk of complications than the initial procedure.
What results can one expect from a knee replacement?
The primary requirement for an artificial knee joint should always be the pain-free management of everyday life. The mobility in the knee is somewhat limited with a prosthesis (bending up to 130°), as the maximum range of motion can no longer be fully achieved for purely mechanical reasons. Sporting activity is generally desirable, but certain things should be taken into account when choosing sports. Sports with high load intensities and with a high risk of injury (contact sports) should be avoided. On the other hand, sports such as cycling, swimming, Nordic walking and hiking are recommended. Depending on previous experience, more demanding sports such as skiing and tennis can be practised again to a certain extent with a knee replacement.
Which knee replacement can be considered for a nickel allergy?
As a rule, knee replacements are made of specially manufactured metal alloys of chromium, cobalt and molybdenum and may also contain traces of nickel. In patients with a diagnosed contact allergy to nickel, this fact must be taken into account, as a reaction could possibly occur. In principle, however, it is not proven that the bone reacts to the allergen (in this case nickel) in the same way as the skin and therefore a nickel allergy is not an absolute reason to exclude a conventional prosthesis made of chrome-cobalt-molybdenum alloys. The skin is of particular importance in immunology because it has to protect the body from external foreign substances and pollutants. For this purpose, specialised immune cells (Langerhans cells) are located in the skin, which are responsible for the immune reaction (or allergic reaction) upon contact with a foreign substance (or allergen). These immune cells and also other biological and biochemical components involved in the immune defence are hardly or not at all found in the bone. Nevertheless, special allergy knee prostheses were made for the case, which are coated with titanium, so that the body does not come into contact with the nickel at all. However, since titanium has a slightly lower sliding ability, there are corresponding disadvantages of the allergy implant (e.g. lower durability). Which knee replacement is finally used must be discussed individually with each patient.